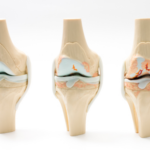
There are four main ligaments of knee.
THESE FOUR LIGAMENTS HOLD THE JOINT STRUCTURE IN PLACE AND PROVIDE SUPPORT. TWO OF THE FOUR LIGAMENTS IN THE KNEE JOINT ARE THE CRUCIATE LIGAMENTS THE KNEE JOINT IS STABILIZED LATERALLY BY THE LATERAL COLLATERAL LIGAMENT, and medialy by medial collateral ligament. THE ANTERIOR AND POSTERIOR CRUCIATE LIGAMENTS ARE LOCATED inside knee.
THE CRUCIATE LIGAMENTS
The front of the tibia is where the anterior cruciate ligament (ACL) attaches and The back of the tibia is where the posterior cruciate ligament (PCL) connect.. Within the knee capsule, the ACL and PCL run in opposition to one another to create an “X.” The ACL resists rotational stress and stops the tibia from moving forward under the femur. The primary stabilizing ligament of the internal knee, the PCL prevents the tibia from moving backward under the femur.
CAUSES OF ANTERIOR CRUCIATE LIGAMENT INJURY
ACL injuries are frequently brought on by improper stress placed on the knee joint. This can happen when the knee joint is turned while the tibia is fixed in place, when there is an immediate shock impact, or when there is a sudden stop or change in direction. The degree of the injury varies; in relatively minor situations, the ligament may just have been stretched out yet still be intact. ACL tears, however, may occur in more severe circumstances. When the ACL is injured, other injuries are frequently present as well, including harm to the menisci, the medial and lateral collateral ligaments, the joint capsule, or the articular cartilage that covers the bones in the knee joint. In addition, the femur and tibia ends may sustain an injury or bruise beneath the cartilage. Additionally, problems like knee osteoarthritis might appear after an ACL tear. ACL injuries may also occur more frequently in women who play sports like football, skiing, and athletic competitions that require twisting, jumping, and landing, according to several studies. This phenomenon may be caused by several things: Women’s intercondylar notches, which are grooves in the femur through which the ACL passes, are thinner than those of men, limiting the ACL’s range of motion, particularly during twisting movements.
• Women’s broader pelvises may have an impact on the quadriceps angle (the angle at which the femur meets the tibia). This changes the knee’s alignment, tending to angle the knee inward (a condition known as valgus alignment), which can increase the strain on the ACL under pressure or twisting.
• Women’s pelvic and femoral muscles are typically weaker than men’s, which causes the knee joint to absorb more force during twisting or sudden movements than the muscles do. Because women’s knees are more pliable than men’s, they are more likely to hyperextend, which puts additional strain on the knee’s muscle fibers and connective tissue. Women can be more vulnerable to ACL injuries at the beginning of their menstrual cycle, before ovulation.
LOWERING THE RISK OF ACL DAMAGE
THE LIKELIHOOD OF ACL INJURY IS INCREASED IF THE MUSCLES ARE NOT WARMED UP BEFORE SEVERE EXERCISE. PEOPLE WHO PARTICIPATE IN ATHLETIC ACTIVITIES HAVE A HIGHER FREQUENCY OF ACL INJURIES.
BY ENGAGING IN WORKOUTS TO INCREASE THE STRENGTH OF CERTAIN MUSCLES AND LEARNING WAYS TO PREVENT INJURY-PRONE CIRCUMSTANCES, THE CHANCE OF ACL INJURY CAN BE SIGNIFICANTLY DECREASED. EXERCISES THAT STRENGTHEN THE PELVIS, THE LOWER ABDOMEN, AND THE LEG MUSCLES ARE BENEFICIAL. TRAINING METHODS FOR THE KNEE POSITION WHILE JUMPING AND LANDING, AS WELL AS TWISTING AND TURNING, ARE ALL VERY BENEFICIAL.
SYMPTOMS OF ANTERIOR CRUCAMENT LIGAMENT INJURY
One of the signs of an ACL injury is the sensation that the knee is giving way when one is bearing weight normally.
• A knee-popping sensation.
• Knee swelling a few hours later.
• Reduction in range of motion and movement.
• Pain during walking.
If you think you may have injured a ligament in your knee, you should follow the “RICE” protocol: rest, ice to minimize swelling, compression bandage application, and elevation of the knee. It is not advisable to completely immobilize the knee because movement helps to reduce stiffness and the risk of muscle atrophy.
CARE FOR ACL DAMAGE
YOUR DOCTOR WILL NEED TO KNOW HOW THE INJURY OCCURRED TO ASCERTAIN ITS CAUSE WHEN THE INJURY IS CLINICALLY EVALUATED.
BODILY EXAMINATION PHYSICAL EXAMINATION PROCEDURES INCLUDE VISUAL INSPECTION, PALPATION, AND EVALUATION OF KNEE JOINT PERFORMANCE. IN ADDITION TO MANIPULATING THE KNEES TO SEE IF THE DAMAGED KNEE ARTICULATES ABNORMALLY, THE DOCTOR WILL EXAMINE BOTH KNEES TO SEE IF THE INJURED ONE IS NOTICEABLY DIFFERENT FROM THE NORMAL KNEE. If an ACL injury is suspected the doctor may perform the ‘Lachman Test’, the ‘Anterior Drawer Test’ or the ‘Lever Sign Test’, to confirm the diagnosis, all of which involve manipulation of the lower leg. Palpation of the joint line can also determine if there is any damage to the lateral meniscus or medical meniscus.Functionality tests determine the stability of the joint and ACL, and can assess any degree of joint separation.
Diagnostic Imaging. X-ray (radiograph) will not show soft tissue such as the ACL, but will often be used to eliminate a break in the bone. An MRI (magnetic resonance imaging) scan would be employed because this will show bone and soft tissue, including any bruising to the bone which might be present.
TREATING ACL INJURY THAT IS PARTIALLY TORN
Because the ACL is made up of bundles of collagen fibers, it is conceivable for the ligament to partially rip with only one bundle being impacted. Partial tear patients can occasionally resume their prior activities without experiencing any weakness or giving way in their knee joint, but for some, the knee will feel unstable and will prevent normal sporting activity. You run the risk of suffering further harm by rupturing other knee structures, such as the medial or lateral meniscus if the knee does seem unstable and you resume your regular sporting activity. Later in life, there is also the added danger of developing articular cartilage lesions.
The difficult decision of whether or not to have surgery is presented by a partial tear. The decision will depend on how much of an ACL was torn, how unstable it was, and whether or not you were an active person. It might be determined that non-surgical treatment of the PARTIAL torn ACL is preferred because the tear is not too restrictive for your way of life and the knee instability is not too bad. However, if instability persists, further injury could occur.
OTHER THAN SURGICAL MANAGEMENT
THE PROGNOSIS FOR NON-OPERATIVE TREATMENT IS FREQUENTLY GOOD, THOUGH A PARTIAL TEAR MAY REQUIRE SEVERAL MONTHS OF RECUPERATION AND THERAPY. ALL THAT MAY BE NEEDED IS A COURSE OF PHYSICAL THERAPY, GUIDANCE ON HOW TO HANDLE INSTABILITY ISSUES, AND PERHAPS ORTHOTIC MANAGEMENT. PHYSIOTHERAPY WOULD BE USED TO HELP THE PATIENT WALK NORMALLY AND RESTORE COMPLETE CONTROL OVER THEIR KNEE. IT IS CRUCIAL THAT THE KNEE CAN UNDERGO FULL RANGE OF MOVEMENT
The prognosis for non-operative treatment is frequently good, though a partial tear may require several months of recuperation and therapy.
MANAGEMENT OF AN ACL RUPTURE
THE LIGAMENT CONNECTING THE FEMUR AND TIBIA HAS COMPLETELY BURST WHEN THE ACL IS ENTIRELY TORN. EVEN WITH PHYSIOTHERAPY, ORTHOTICS, AND THE POTENTIAL FOR A LIFESTYLE ADJUSTMENT, IT’S POSSIBLE THAT THE RUPTURE STILL LEAVES AN INSTABILITY THAT LOWERS THE QUALITY OF LIFE. WITHOUT SURGICAL INTERVENTION, PATIENTS WHO HAVE AN completeACL TEAR ARE TYPICALLY ADVISED TO HAVE SURGERY.
ACL IN CHILDREN
Because children and teenagers have not yet attained skeletal maturity and there is a risk of damaging their growth plates, it has been thought—and is still thought—that surgery should not be advised in these cases. The necessity for meniscal surgery and treatment for cartilage defects, however, may have resulted from non-operative treatments, according to recent theories. Additionally, there have been instances of persistent instability and unsuccessful results. Today, many pediatric orthopedic doctors would advise surgical repair for kids who had an ACL tear confirmed by the pivot shift test, which rotates the tibia and femur to check for instability and gauge the severity of crippling knee dysfunction.
SURGERY-GRAFTS FOR ACL
ACL RIPS CANNOT BE STITCHED TOGETHER. INSERTING A GRAFT IS A COMMON SURGICAL OPERATION. TO INTRODUCE THE GRAFT INTO THE KNEE JOINT AND SECURE IT, TUNNELS ARE drilled THROUGH THE FEMUR AND TIBIA. LIGAMENT GRAFTS ARE DERIVED FROM THE PATIENT’S TISSUE. A SYNTHETIC TUBULAR GRAFT IS AN ALTERNATIVE.
Allografts are discouraged since there is a risk of disease spreading during the procedure. Additionally, it’s occasionally believed that the allografts that are given by numerous companies and that have been chemically and radioactively treated tend to degrade over time. Furthermore, compared to autografts, certain research indicates that allografts have a higher failure rate. Allografts, on the other hand, is gaining popularity and do offer the benefit of doing away with the discomfort connected with autograft harvesting. Additionally, they require fewer incisions and the surgeon can graft them more quickly. When patients require multiple knee ligament reconstruction or revision surgery, allografts and synthetic grafts are frequently employed. In the case of autografts various tendons could be used including the quadriceps, patellar and hamstring tendons, with the hamstring tendons often being favoured.
The center third of the patellar tendon can be used to create a new ACL. On one end of this graft, a bone plug from the patella was used, and on the other, a plug from the tibia. These bone plugs serve as a seating area for the graft. However, employing this transplant does seem to increase the likelihood of postoperative discomfort below the knee.
Specialists frequently believe that hamstring tendon grafts are preferable, which is why they are growing in popularity. They contend that they have fewer adverse effects than patellar tendon grafts and that they are also simpler to harvest. Patients can leave the hospital a few hours after the procedure because it is a day care surgery and they are always able to bear their weight right away.
For surgical ACL reconstructions, synthetic ligaments were created in the 1980s and 1990s; the third generation of these materials is currently available. A flawless synthetic graft has not yet been discovered, despite numerous efforts using materials including carbon fiber, Dacron, and PTFE (Polytetrafluoroethylene). Other artificial ligament types are still being worked on.
REHABILITATION FROM ACL SURGERY
THE REPLACEMENT OF THE LIGAMENT IS SIMPLY ONE STEP IN THE PROCESS; A FULL RECOVERY COULD TAKE OVER A 45 to 50 days. THE FRAME OF THE REPAIRED LIGAMENT WILL BE PUT IN PLACE DURING ACL SURGERY, BUT THE BODY MUST PHYSIOLOGICALLY TRANSFORM THIS FRAMEWORK OF TENDONS INTO A WORKING LIGAMENT. AS THE HEALING GRAFT UNDERGOES THE BIOLOGICAL AND MECHANICAL CHANGES KNOWN AS LIGAMENTIZATION, THE PATIENT MAY FEEL WEAKNESS AND DECREASED FUNCTION IN THE KNEE JOINT. THIS IS A TYPICAL STEP IN THE PROCESS AND IS NOT CAUSE FOR CONCERN.
BEFORE THE OPERATION
Before surgery, patients must complete important tasks that will ensure a successful procedure and a speedy recovery afterward. The preoperative period may be weeks or months because before surgery can be performed, all swelling must have gone down and a full range of motion must be recovered. Additionally, to strengthen the quadriceps and hamstrings, the patient should engage in some low-impact exercise, such as swimming, cycling, or the gym; running and jumping should be avoided. The patient should also undergo some physiotherapy. Strengthening muscles at this point will improve recovery from surgery quicker, and easier, and give the greatest chance possible. Physiotherapy exercises learned now will aid with post-operational exercises.
REHABILITATION
THE REHABILITATION PROCESS IS DIVIDED INTO SIX STEPS. EACH STEP IS GIVEN AN APPROXIMATE TIME AFTER THE OPERATION, HOWEVER GOALS RATHER THAN TIME SHOULD BE USED TO MEASURE THE STAGES. THE RETURN TO REGULAR FUNCTIONING IS THE ULTIMATE GOAL.
STAGE 1. IMMEDIATELY POST OPERATION TO 14 DAYS AFTER THE OPERATION
The benefits of immediate mobilization and as much weight bearing as is comfortable following surgery. Bruising, swelling, and redness at the site of the injury are common and should be treated with ice and leg elevation because the wound will be healing. The objectives for this stage include full weight bearing on the leg and joint range of motion. To assist restore coordinated muscular function, gentle activities that target both the hamstring and the hamstring/quadriceps muscle groups simultaneously are started. Goals include less usage of crutches and a return to regular walking motion, as well as the beginnings of muscular control and the capacity to completely extend the limb.
STAGE 2: 2 TO 6 WEEKS FOLLOWING THE PROCEDURE
EXERCISES EMPHASIZE THE DEVELOPMENT OF STRONG MUSCLE CONTROL, ESPECIALLY IN THE QUADRICEPS AND HAMSTRINGS. THE LENGTH AND VARIETY OF THESE ACTIVITIES ARE INCREASED. WORK BEGINS TO ASSIST THE PATIENT IN BECOMING CONSCIOUS OF THE LOCATION OF THE KNEE AND IN REGAINING BALANCE AND JOINT STRENGTH. MORE WORK IS PUT IN TO ACHIEVE A RETURN TO NORMAL WALKING ACTION IF IT HAS NOT ALREADY BEEN DONE SO. ANY PERSISTENT JOINT SWELLING CAN BE TREATED WITH A COLD COMPRESSION KNEE WRAP.
STAGE 3: SIX TO TWELVE WEEKS FOLLOWING THE OPERATION.
EXERCISES FOR THE SENSORS THAT MEASURE A JOINT ANGLE, MUSCLE TENSION, AND JOINT POSITION IN SPACE ARE THE MAIN EMPHASIS OF THE WORK. OTHER OBJECTIVES INCLUDE STARTING WORK ON NEUROMUSCULAR CONTROL TO RETRAIN MOVEMENT PATTERNS AND SKILLS AND ENGAGING IN LEG MUSCLE TRAINING TO INCREASE STAMINA, STRENGTH, AND SELF-ASSURANCE.
STAGE 4. FROM 12 WEEKS TO 5 MONTHS AFTER THE OPERATION
The main goal is to enhance neuromuscular performance. All of the leg muscles are still being strengthened, and agility is being added. Exercises are combined with the agility to enhance the perception of joint movement in space. The program introduces skills that will allow the patient to resume sporting activities, and confidence is boosted.
STAGE 5. FROM 6 TO 12 MONTHS AFTER THE OPERATION
This phase focuses on continuing to get ready for a comeback to sports, which includes honing methods and skills and enhancing confidence, strength, and endurance. Exercises involve stretching and tightening the muscles quickly and repeatedly, strengthening the muscles, and enhancing agility.
STAGE 6, AFTER TWELVE MONTHS OF THE OPERATION
THE THIRD STAGE INVOLVES RETURNING TO ATHLETIC ACTIVITY WHILE TAKING PRECAUTIONS, SUCH AS WARMING UP WITH NEUROMUSCULAR ACTIVITIES THAT SIMULATE UPCOMING BODY MOTIONS. THE NEUROMUSCULAR PROGRAMME IS CONTINUED, AND A CAUTIOUS APPROACH IS TAKEN WHEN REINTRODUCING FULL ATHLETIC ACTIVITY.